tPA a plasminogen activator used in HIV Drug Treatment could improve recovery after stroke
A protein that may hinder the brain’s regrowth after damage points researchers to an unexpected treatment
Stroke treatment has been a race against time. In the hours after a stroke, the clot-busting treatment tissue plasminogen activator (tPA) can limit damage to the brain. But once that damage is done, no drugs are known to promote recovery. New research suggests such a therapy could come from an unlikely target: a cellular protein called CCR5 that allows HIV to infect cells. Scientists found that in mice, disabling CCR5 helps surviving neurons make new connections, and that people who carry a CCR5 mutation may recover better from a stroke.
“This is the first real molecular target to improve recovery after stroke,” says Argye Hillis, a stroke neurologist at Johns Hopkins University School of Medicine in Baltimore, Maryland, who was not involved in the work. A clinical trial will soon test its promise by giving stroke patients an HIV drug that blocks CCR5.
White blood cells display CCR5 on their surface to intercept signals from molecules called chemokines and coordinate an immune response. But HIV exploits CCR5, grabbing onto it to invade host cells. People with a mutation that cripples the CCR5 gene are protected from infection, which is why Chinese scientist He Jiankui recently aimed to mutate CCR5 in controversial human experiments.
The new discoveries about CCR5 began with a hunt for “smart mice”—animals bearing genetic mutations that apparently boost their ability to learn and remember. Neuroscientist Alcino Silva and his team at the University of California, Los Angeles (UCLA), wanted to figure out which of 148 mouse strains had such enhancements. In 2016, they reported that reducing levels of CCR5 in a healthy mouse brain enhanced memory formation and learning.
UCLA stroke neurologist Thomas Carmichael was intrigued. “When you watch patients recover in stroke, it looks like they’re relearning to walk or relearning language,” he says. Indeed, surviving neurons near the injury sprout tendrils to make new contacts across the brain. A drug that targets CCR5 seemed promising for stroke recovery, and that drug was already on hand. Maraviroc, which blocks CCR5, was approved by U.S. regulators in 2007 for use with other antiretroviral drugs to treat HIV infections.
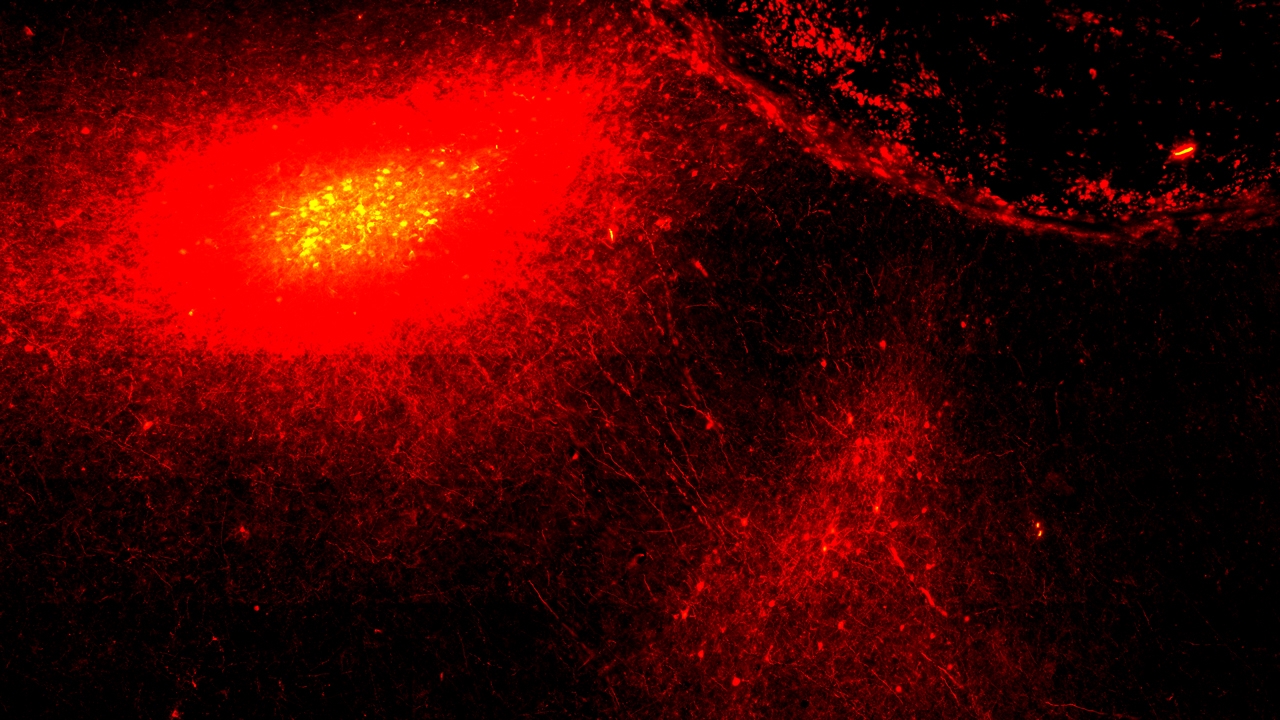
In Cell this week, Silva, Carmichael, and their collaborators showed that CCR5 levels in mouse neurons skyrocket after stroke and can remain elevated for weeks—and that the protein appears to hamper recovery. The team blocked CCR5 with maraviroc or a gene that interferes with its production, and then ran the mice through tests of motor ability—for example, counting how many times their feet slipped as they walked across a metal grid. Treated mice showed greater motor improvements than controls at the end of the 9-week testing period.
Even if the researchers waited until 3 weeks after a stroke to give the animals maraviroc, it improved their performance. In previous studies, nothing has seemed to help at that point, says Dale Corbett, a neuroscientist specializing in stroke recovery at the University of Ottawa. The new results, he says, suggest “it may be feasible to reopen this recovery window in people.”
Blocking CCR5 seemed to help maintain connections between neurons adjacent to the injured site. And it caused neurons in motor regions to sprout more projections to the opposite side of the brain, a process that might help a mouse relearn lost movements.
What CCR5 does in the poststroke brain is hazy. Surging CCR5 is part of the inflammatory response to stroke, says Robyn Klein, a neuroimmunologist at Washington University School of Medicine in St. Louis, Missouri. In flammatory molecules may prompt neurons to express more of this chemokine receptor. In the developing brain, chemokines are known to influence how neurons migrate and connect. After stroke, they seem to decrease the number of connection sites on neurons near the damage. (How that process hinders regrowth and recovery isn’t clear.)
Carmichael notes that blocking CCR5 also caused neurons to express genes that increase their excitability, making them fire more readily. He suspects that neurons boost CCR5 after a stroke to dampen their activity and lie low to avoid a deadly cellular frenzy known as excitotoxicity. But because the protein then sticks around, that protective mechanism gets in the way of recovery.
Mouse results often prove meaningless in people, but when Carmichael’s group teamed up with researchers behind the Tel Aviv Brain Acute Stroke Cohort (TABASCO) in Israel, they found encouraging clues. Roughly 10% of Europeans have a genetic deletion that cripples CCR5, and the number is higher in Jewish people of Eastern European origin. The TABASCO team identified 68 people in its cohort of stroke survivors who had at least one copy of the CCR5 mutation. Compared with people without the mutation, they performed slightly better on tests of motor and sensory skills and cognitive abilities both 6 months and 1 year after a stroke, the new study found.
“It wasn’t gangbusters better, but … the fact that they found anything is impressive,” says Steven Cramer, a stroke neurologist at UC Irvine, who has studied genes linked to stroke recovery.
Carmichael and his collaborators are now designing a clinical trial that will give 30 people maraviroc starting when they leave an inpatient rehabilitation facility—typically about 4 weeks after a stroke. The team hopes to launch the trial this year.
Meanwhile, some researchers expect the CCR5 story to inspire a broader search for brain repair strategies based on learning and memory genes. “We’ve always been talking about having a tPA-like moment for stroke recovery,” Corbett says. “Whether this is it or not, I don’t know, but at least it gives us hope.”