Can You Reverse Coronary Artery Disease?
The Power of Lifestyle
Lifestyle changes alone likely aren’t enough when you have coronary artery disease, but there’s no doubt that they’re a powerful addition to medication, Foranow says.
The American Heart Association recommends a diet that’s rich in:
- Fruits and veggies
- Whole grains
- Low-fat dairy products
- Skinless poultry and fish
- Nuts and legumes
- Non-tropical vegetable oils like olive oil
You should also limit saturated fat, sodium, red meat, and sweets.
A nutrition plan created by Dean Ornish, MD, has been shown in small studies to lower cholesterol and reverse CAD. Ornish’s diet requires you to follow a mainly plant-based eating plan that focuses on whole grains, fruits, vegetables, legumes, and soy products, with the option of nonfat dairy and egg whites. The plan is very low in fat, limiting fat to about 10% of your total calories. That can be very hard to stick to, says Fonarow. “We want to encourage people to make dietary changes that they’ll be able to stick with long-term,” he says.
Other parts of a healthy lifestyle won’t necessarily reverse coronary artery disease but may prevent it from getting worse. These include:
- Regular exercise. Regular physical activity helps repair some of the damage in the endothelium, the thin membrane that lines the inside of blood vessels. This, in turn, allows more blood to pump through your vessels.
- Not smoking. Cigarette smoke causes the platelets in your blood to become stickier and clump together, which can lead to a blood clot that can cause a heart attack.
- Stress management. If you’re too stressed for too long, it can be a problem. Chronic high levels of stress hormones such as cortisol raise blood cholesterol and also cause changes that promote the buildup of plaque in your arteries. There are many ways to manage stress, including exercise, keeping up close social ties, talking with a therapist, and meditation. Studies show that people who meditate regularly are about half as likely to get coronary artery disease as those who don’t.
“Taken together, all these steps can help lower your risk of having a heart attack or stroke,” Nissen says. “Our goal is to keep you alive and healthy,” even if your coronary artery disease doesn’t fully reverse.
Can we reduce vascular plaque buildup?
The key is lowering LDL and making lifestyle changes.
High blood levels of cholesterol encourage the formation and growth of vascular plaques that put you at risk for heart attack and stroke. So, can we reduce plaque buildup? “Making plaque disappear is not possible, but we can shrink and stabilize it,” says cardiologist Dr. Christopher Cannon, a Harvard Medical School professor.
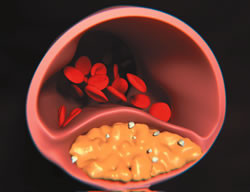
Plaque forms when cholesterol (above, in yellow) lodges in the wall of the artery. Image: Thinkstock |
What causes plaque in arteries?
Plaque forms when cholesterol lodges in the wall of the artery. To fight back, the body sends white blood cells to trap the cholesterol, which then turn into foamy cells that ooze more fat and cause more inflammation. That triggers muscle cells in the artery wall to multiply and form a cap over the area. But the soft plaque beneath the cap is dangerous. “For example, if your blood pressure spikes, it puts pressure on the thin wall of the plaque, which can break open, form a clot, and cause a heart attack,” says Dr. Cannon. About three of every four heart attacks occur when plaques rupture.
Larger plaques can block blood flow. But they are typically covered by thick, fibrous caps that can resist breaking apart. These are often treated by inserting a wire mesh tube (stent) near the blockage to widen the artery.
Treatment for plaque buildup
Doctors target smaller, unstable plaque. “If we have a 30% blockage in the artery from soft plaque, the goal is to try to suck out the cholesterol from the inside, so the plaque shrivels down to 15% and leaves nothing inside it,” says Dr. Cannon.
How do you get the cholesterol out of the plaque? By lowering levels of cholesterol in the blood, where it travels inside particles called lipoproteins. Low-density lipoprotein (LDL) deposits cholesterol into blood vessel walls. The drugs used most often to reduce LDL cholesterol levels are statins—such as atorvastatin (Lipitor) and rosuvastatin (Crestor). Statins block the liver enzyme that promotes cholesterol production. Another medication called ezetimibe (Zetia) may be added to inhibit the absorption of cholesterol in the digestive tract. “Shrinking plaques with strong statins has been seen when you get LDL below 70 (mg/dL),” says Dr. Cannon. Harvard Health Letter
Science has proven that chronic, low-grade inflammation can turn into a silent killer that contributes to cardiovascular disease, cancer, type 2 diabetes and other conditions. Get simple tips to fight inflammation and stay healthy — from Harvard Medical School experts.
Very intensive lifestyle changes have also been shown to shrink plaque. Dr. Cannon recommends that you:
- Eat a Mediterranean diet.It can reduce heart disease risk by 30%. It is rich in olive oil, fruits, vegetables, nuts and fish; low in red or processed meats; and moderate in the amounts of cheese and wine you can consume.
- Kick the habit.Smoking damages the lining of the arteries. Quitting can help raise HDL levels.
- Exercise.Aerobic exercise can raise HDL, lower blood pressure, burn body fat, and lower blood sugar levels. Exercise combined with weight loss can also lower LDL levels. Aim for 150 minutes per week of moderate-intensity exercise.
Busting the cholesterol mythWhy you can’t live without this tricky substance. Cholesterol is often vilified as the bad guy, but we need this waxy, fatty substance to make vitamin D, hormones, bile that aids digestion, and the coverings of our cells. The liver produces 75% of the body’s cholesterol, but all cells have the ability to make it. When cells need more cholesterol, the liver sends it via the bloodstream in packages made of cholesterol on the inside and protein on the outside. These cholesterol-laden particles are known as low-density lipoprotein, or LDL. Too much LDL in the blood can cause cholesterol to lodge in the artery walls and form plaques. That’s why LDL is known as “bad” cholesterol. Not surprisingly, high levels of cholesterol in the diet raise blood levels of LDL. But high levels of saturated fat and trans fat in the diet are even more important: they cause the liver to produce lots of LDL cholesterol and send it into the blood. Whereas LDL particles deposit cholesterol into plaques of atherosclerosis, some high-density lipoprotein (HDL) particles help remove cholesterol from plaques. That’s why it’s often referred to as “good” cholesterol. How much HDL and LDL should you aim for? An HDL of 60 milligrams per deciliter (mg/dL) or greater is associated with a lower risk of heart disease. Many doctors prescribe statins and lifestyle changes to get LDL levels below 70 mg/dL in people at high risk of having a heart attack in the next 10 years. Recent guidelines recommend that statins be prescribed regardless of the LDL level in people at high risk of heart attack because of cardiac risk factors (such as high blood pressure, diabetes, and smoking). |
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.

