Frostbite
What is frostbite? How cold does it need to be to get frostbite and how fast does it occur?
How to avoid skin injury during extreme weather in the US this week
As chilly Arctic air takes over the eastern US during a “bomb cyclone“ over the coming days, bringing powerful winds snow and ice with it, residents will be at higher risk of frostbite.
Here’s what to know about the skin injury caused by extremely low temperatures and how to avoid it:
What is frostbite?
Frostbite is when the skin and tissue freezes. It most commonly affects the most exposed parts of the body, including fingers and toes, plus the nose, ears, and face. It starts with numbness due to the cold and is often accompanied by a red colour on paler skin, followed by blisters and swelling. It can permanently damage limbs as blood flow is restricted from extremities in order to send it to the vital organs. The parts of the body with less blood will get colder and the moisture in the tissue can freeze into ice crystals.
Frostbite is skin damage caused by freezing temperatures below 32 degrees Fahrenheit (0 degrees Celsius). You’re more likely to get frostbite in any situation that leads to prolonged cold exposure:
- During the winter.
- In windy weather conditions.
- At high altitudes.
- If you don’t have shelter from the cold weather.
You can get frostbite even under cold-weather clothing.
Frostbite may lead to permanent, irreversible tissue damage (necrosis). A way to prevent frostbite is to limit your time outdoors and warm up your body often if you’re exposed to freezing temperatures.
If you believe you have frostbite, go inside or seek shelter from the cold. Then, call your healthcare provider or visit the emergency room immediately to reduce your risk of tissue damage.
When does it happen?
Wind chills of around -27°C (-17°F) or more can cause frostbite to occur quickly – in less than 30 minutes. However, it can occur at -0.55°C (31°F) over longer periods of time. You cannot get frostbite above freezing temperature degrees (0°C/32°F), but you can get still get hypothermia – which happens when your body temperature goes below 35°C (95°F) degrees.

How serious is it?
Frostbite can occur in several stages, from mild to very serious. Mild symptoms include numbness, reddish skin, mild pain and pins and needles – this is a warning sign you need to get somewhere warm. Blisters will appear in more serious superficial frostbite, and the skin may even feel warm.
Severe frostbite affects all layers of the skin and the tissue below. In severe cases, those affected by frostbite may not even know they have it – as they will stop feeling pain and stop feeling the cold temperature on the areas affected.

Those with lighter skin may notice a blue-grey colour. Extremities without blood flow may die and surgery may be needed to remove the dead tissue. Amputation of limbs may be needed if frostbite is severe.
How can I avoid getting it?
Keep sheltered and keep warm. If you do have to brave the elements, make sure you are dressed warmly with plenty of layers (including those on the most vulnerable areas – so balaclavas, thick gloves, warm waterproof boots etc) and don’t spend prolonged periods of time in the cold. If you are stuck in the cold, keep moving to generate heat.
Older adults and babies are more at risk of frostbite, as are homeless people, hikers and hunters.
What do I do if I get frostbite?
Seek medical help immediately. Try not to touch, massage or itch your frostbite as it will remove the skin and could cause permanent damage. Do not walk on frostbite-affected feet.
Until help arrives, try to find a warm – not hot (no fires) – place. When there, remove all wet clothing and put warm clothes/blankets on. Do not place anything hot on frostbite, it needs to warm up gently. Warm water can help (bath of water at 37°C to 39°C (98.6°F to 102.2°F). The warming process can be painful – medical professionals will likely prescribe strong painkillers.
Who does frostbite affect?
Frostbite can affect anyone with exposure to cold temperatures. It’s most common on your fingers, toes, nose and ears. You’re more likely to get frostbite with prolonged cold exposure, especially if you:
- Are younger than 18 years of age or are over 65 years of age.
- Live and work in cold climates.
- Are without housing.
- Have an underlying medical condition like peripheral vascular disease, malnutrition, Raynaud’s syndrome, hypothyroidism, arthritis or diabetes.
- Smoke tobacco products.
How common is frostbite?
Frostbite is common, but it’s less common than it used to be. This is because people have better access to cold-weather clothing and know more about the dangers of frostbite and how to prevent it.
What are the stages of frostbite?
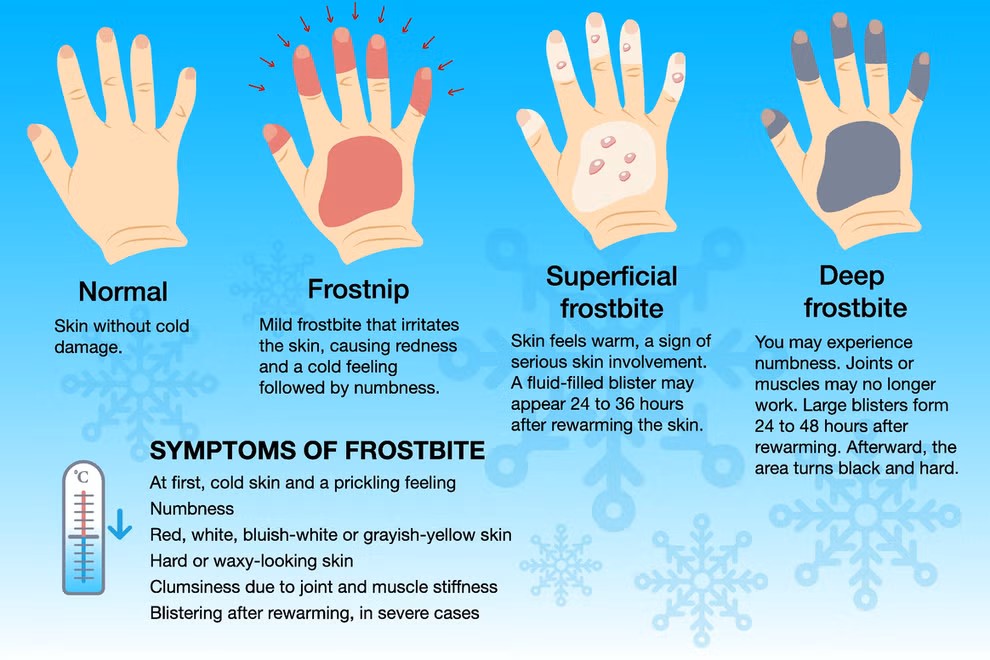
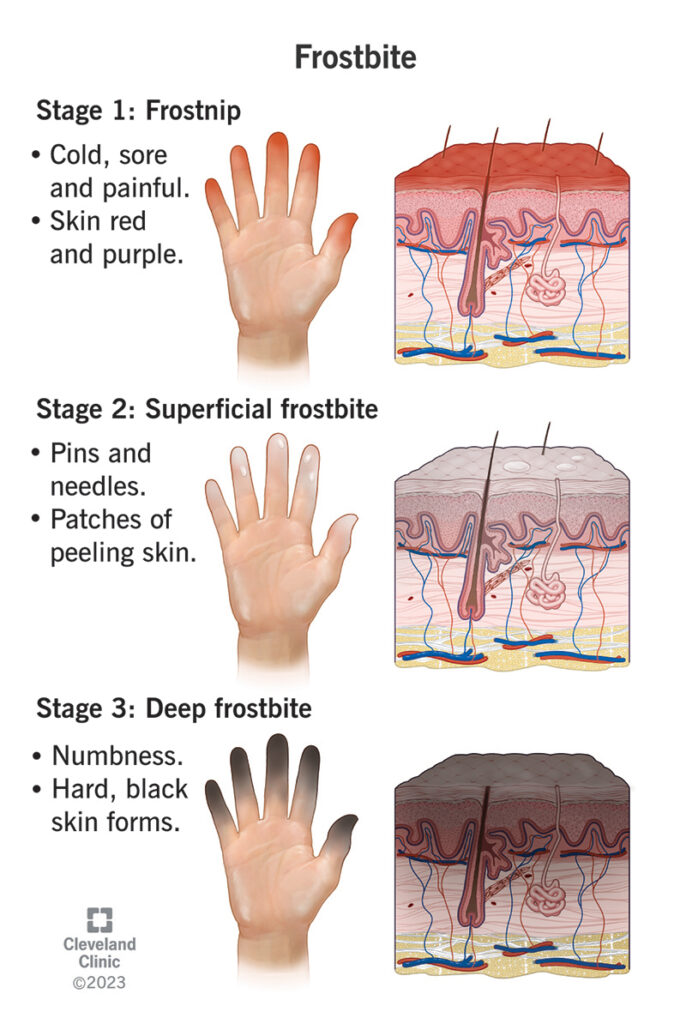
Frostbite symptoms appear in three stages that include feeling:
- Cold, sore and painful (frostnip).
- Pins and needles (surface frostbite).
- Numbness (deep frostbite).
If you notice any of the symptoms of the second or third stages of frostbite, get immediate medical treatment to prevent long-lasting damage.
Symptoms and Causes
What does frostbite look and feel like?
Symptoms of frostbite vary based on what stage you’re in and the severity of skin damage that the cold caused.
- Frostnip: During frostnip or the first stage of frostbite, you may see that your affected skin is red to purple or lighter than your natural skin tone. Your skin may also feel cold, slightly painful and tingly. Frostnip is the warning stage when skin damage is just temporary. If you notice symptoms, get inside immediately and thaw the affected area of skin with warm (never hot) water. Afterward, you may notice small red bumps (chilblains) on your skin. Even if you have mild symptoms, visit a healthcare provider to make sure you don’t have long-term damage from frostnip.
- Superficial (surface) frostbite: This is the second stage of frostbite, and it requires medical treatment. Your skin might feel warm, but the water in your skin is slowly freezing into ice crystals. Your skin contains over 60% water. This can cause a “pins and needles” feeling. In addition, your skin may sting or swell up. After rewarming, you might have painful, spotty patches or purple or blue areas of skin like a bruise. Your skin might start to peel and feel just like a sunburn. You may also get fluid-filled blisters in the area after a day or so.
- Severe (deep) frostbite: In the third stage of frostbite, your lower layers of skin (subcutaneous tissue) freeze and total numbness sets in. It can be difficult to move the area that’s frostbitten or you may not be able to move it normally. Get medical attention immediately if you experience any of these symptoms. Big blisters will appear on the frostbitten skin a day or two after cold exposure. Your frostbitten skin turns black because your skin cells die after freezing. Your skin might form a hard, black covering (carapace) that falls off on its own. If it doesn’t, a healthcare provider will remove it surgically.
Frostbite is dangerous because it often numbs your skin so you may not feel that anything’s wrong at all. Contact a healthcare provider if you believe you have frostnip or frostbite.
Can you have frostbite and not know it?
Yes. Many people who get frostbite are completely unaware that they have it. This happens because frostbite numbs your nerves and can cause damage deep inside your skin. You might not notice any symptoms after coming in from the cold. It’s important to limit your time outdoors in freezing temperatures to prevent frostbite.
Where are common places to get frostbite?
Frostbite can affect any part of your skin, but you’re more likely to get frostbite on your extremities. These are parts of your body that are the most exposed to cold temperatures, even if they’re bundled up and include your:
- Hands and fingers.
- Feet and toes.
- Face and nose.
- Ears.
How do I know if my child has frostbite?
It can be difficult to tell if your child has frostbite. Infants don’t shiver like adults because they don’t have as much energy stored up. Older children are usually too busy having fun outside to notice they’re frostbitten.
If your baby or toddler is outside in the cold for even 10 minutes, it’s time to check on them. If you notice parts of their skin are lighter than their natural skin tone, red, white or gray, contact their healthcare provider.
If your children are older and they’ve been outside for more than half an hour in freezing temperatures, even with cold weather clothing on, ask them to come inside and remove their wet clothing. They should put on dry clothes and warm their body under blankets. A warm bath may also help your child warm up from the cold. Always use lukewarm, never hot, water.
How do you get frostbite?
Freezing temperatures cause frostbite. Cold temperatures (slightly above freezing) for long periods of time can also cause frostbite. You can get frostbite by:
- Exposure to freezing temperatures.
- Having frozen objects like an ice pack or metal pressed against your skin.
- Not wearing sufficient clothing to protect your skin from the cold.
Even if you’re wearing protective clothing like a hat, boots and gloves, you can still get frostbite through your clothing.
When you get frostbite, the water within your skin freezes and crystalizes. Over 60% of your skin contains water. This damages your skin cells and tissues, which prevents blood flow to these areas of your body. Severe frostbite can damage your muscles, nerves and joints.
How long does it take for you to get frostbite?
You can get frostbite in 30 minutes or less when the wind chill is -15 F (-26 C) or lower. If you live or work in cold climates, try to limit your time outdoors to prevent skin damage.
How cold does it have to be to get frostbite?
Freezing temperatures cause frostbite. It needs to be colder than 32 F or 0 C for you to get frostbite. Remember that the temperature may be significantly colder if there’s wind, which can increase your risk of getting frostbite.
Diagnosis and Tests
How is frostbite diagnosed?
A healthcare provider will diagnose frostbite after a physical exam and possible imaging tests. During your exam, your provider will look for skin discoloration or other skin symptoms like mottling or blisters. Your provider will also ask you questions about your cold exposure. For example, how long were you exposed to freezing temperatures and what was the temperature during exposure?
Depending on the severity of your symptoms, your provider may take an imaging test like an X-ray to look beneath your skin for tissue damage.
What’s a sign of permanent skin damage from frostbite?
Your healthcare provider will let you know whether or not your skin damage is permanent. An indication that you have temporary skin damage is the presence of clear blisters. If you have blood-filled blisters, you may have permanent damage. If your skin turns black or darker than your natural skin tone, that’s a sign of severe tissue damage. In that case, you may need surgery to remove your damaged skin to prevent secondary infections or gangrene.
Management and Treatment
How is frostbite treated?
Treatment for frostbite varies based on the stage.
If you show signs of frostnip, go indoors or find shelter to get out of freezing temperatures, if possible. Next, take these steps to warm your affected skin:
- Gently remove your cold weather gear, like gloves or boots. You should also remove any jewelry like rings or watches if they’re near an affected area of skin. If your clothing is wet, put on dry clothing.
- Place your affected skin in a bath of warm (not hot) water. This will be a slow rewarming process that can take at least 30 minutes.
- Place blankets on your affected area of skin. Don’t wrap blankets around your skin because it could cut off circulation and prevent blood flow to your affected tissues.
- Avoid applying heat directly to your skin to prevent burns.
If you have signs or symptoms of surface or deep frostbite, which are the second and third stages of frostbite, visit a healthcare provider immediately for treatment. Time is critical with frostbite. You may experience severe pain with frostbite as your skin thaws.
To treat frostbite, a healthcare provider will:
- Raise your body temperature in lukewarm water or by applying warm, wet packs to your skin for up to 30 minutes.
- Apply wound dressings to your frostbitten skin with sterile bandages, keeping your fingers and toes separated to avoid rubbing.
- Test blood flow in the affected area of your body. If you have stage three frostbite, your provider may also connect you to an IV (a needle that enters a vein in your arm to deliver fluids) to improve your circulation.
- Give you antibiotics and pain relievers, such as ibuprofen (Advil®, Motrin®).
- Rehydrate your body by giving you water (frostbite dehydrates your tissues).
- Give you oxygen therapy. For extreme frostbite, your provider may have you breathe pure oxygen inside a pressurized room. This treatment, called hyperbaric oxygen therapy, helps some people heal faster by increasing their blood-oxygen levels.
Do I need surgery for frostbite?
For severe cases of frostbite, your provider may need to perform surgery to remove any dead skin and tissue after you heal. It may take days or even months to determine if you need surgery. Surgeons may need to remove (amputate) the fingers or toes if your tissue died or if you develop gangrene.
Can I treat frostbite at home?
You should seek care from a healthcare professional if you have frostnip or frostbite. If you’re in a remote area or you’re unable to go to the hospital right away, you can take steps to treat frostbite at home to prevent it from damaging your skin and tissues. Your priority is to make sure you stay warm. You should find shelter and prevent warming and refreezing of your body, which can cause more severe skin damage. To warm up, follow these steps:
- Remove all wet clothing and put on dry clothing.
- Elevate the injured area slightly.
- Warm your skin by soaking the frostbitten area in warm water, around 98.6 F to 102.2 F (37 C to 39 C). It can be difficult to determine the temperature of the water, as your skin may be numb. Use a thermometer if you have one available. When your skin feels soft again or after at least 30 minutes, you can stop warming it.
- Cover your frostbitten area with a clean cloth. If your fingers or toes are frostbitten, wrap each one individually. Make sure you keep them separated to avoid stress or pressure. Avoid tightly wrapping your fingers and toes to allow blood to circulate easily.
- Try not to move the area at all while you’re thawing. Avoid walking on frostbitten toes or feet.
- Don’t rub frostbitten areas because rubbing skin that’s hard or numb can cause tissue damage.
You may experience pain during the thawing process. This is normal. You may take over-the-counter pain relievers as directed by your healthcare provider.
Prevention
How can I prevent frostbite?
Here are a few tips for preventing frostbite:
- Avoid going outside: When it’s cold out, try to stay indoors.
- Limit your trips: If you do have to go outside, try to limit it to 10 or 15 minutes before going back inside for a few hours.
- Dress warmly before going out: Dress appropriately whenever you know you’re going to be in cold temperatures. Layer your clothing. Wear warm socks, a thick hat, mittens and a heavy scarf over your face, ears and mouth.
- Wear windproof and waterproof clothing: Wear clothes designed to keep the weather out and to keep your head and neck area warm.
- Don’t cut off your circulation: Make sure your boots and clothes aren’t too tight. This can cause poor circulation. Keep moving to maintain a good blood flow.
When traveling in cold weather, always bring your phone with you. It’s your lifeline to medical help if you have an accident or get stuck on the road. Finally, pack a car emergency kit in your vehicle. That way, you’re prepared with first aid, food and water, gloves, boots and blankets whenever the weather turns bad.
Outlook / Prognosis
What can I expect if I have frostbite?
If you think you have frostbite, go inside and contact a healthcare provider or visit the emergency room.
The amount of time it takes after treatment for your frostbitten skin to feel better depends on which stage of frostbite you were in and for how long. If you have very mild frostnip, you may heal within a few days to a few weeks. Second-stage frostbite can take up to six months for your skin to heal. You may experience skin scabbing and skin discoloration throughout the healing process. The third and most severe stage of frostbite can cause permanent skin damage. You may need surgery to repair this type of skin damage. A healthcare provider can give you the best timeline of when you can expect your skin to heal based on the severity of your symptoms.
What are the complications of frostbite?
Complications from frostbite are possible. When frostbite continues past the first stage (frostnip), it can have long-term side effects including:
- Nerve damage (neuropathy).
- Sweating heavily.
- Being more sensitive to the cold.
- Frostbite arthritis, stiffness in your hands and feet.
- Skin discoloration.
- Nail damage or nail loss.
- Scarring.
You’re also more likely to get frostbitten again once it’s happened.
Severe complications of frostbite can include:
- Gangrene.
- A secondary infection.
- Amputation.
- Damage to your tendons, muscles and bones.
Living With
When should I see a healthcare provider?
If you think you have frostbite, don’t wait to seek help. Immediately contact a healthcare provider or visit the emergency room. Acting quickly and removing yourself from freezing temperatures can prevent severe complications.
What questions should I ask my doctor?
- What stage of frostbite do I have?
- Will I have long-term damage from frostbite?
- How do I take care of my skin as it heals?
- Do I need surgery to treat frostbite?