Gabapentin & Stroke recovery: How an existing drug may help the brain repair itself after stroke
New research in mice shows how doctors may be able to use an anticonvulsive drug to help the brain heal
- The brain can often find new ways to route signals around damaged areas to restore lost function.
- A new study in mice finds that administering a common drug soon after a neurological event can help the brain successfully rewire itself.
- If further research validates the study’s conclusions, physicians may have a new tool for preventing permanent stroke damage.
Dr. Andrea Tedeschi, assistant professor in the Department of Neuroscience at Ohio State University Medical Center, explained to Medical News Today why the concept of “brain plasticity” is so important when it comes to understanding brain health:
“‘Brain plasticity’ refers to the innate, or intrinsic, ability to compensate for a lack of functioning areas by, in principle, rewiring spare areas of the nervous system. And it’s something that is really amazing if you think about it because it allows us to repair the nervous system under certain conditions.”
Dr. Tedeschi is the corresponding author of a new study in mice that investigates the use of an existing drug to help the brain repair itself after an ischemic strokeTrusted Source.
The study found that administering gabapentin, an anticonvulsive medication, soon after a stroke helps the brain more effectively work around damaged areas.
Dr. Tedeschi explained: “I think that the way that the drug is [commonly] being prescribed, it’s to deal with the consequences of […] maladaptive changes [that] are now intrinsically wired into the system. So prescribing the drug if [the patients] have some sort of pain or [problematic] excitability of a certain part of the brain […] it’s not going to wipe [it] out.”
By contrast, “[t]he way we intend to use it,” Dr. Tedeschi said, “it’s more or less as a prophylactic type of drug.”
“Administering this class of drugs in an earlier phase, when the system has not yet committed to a maladaptive route, then I think it’s really increasing the chances of something that we call an adaptive response.”
The study appears in BRAIN.
Gabapentin blocks two proteins, alpha-2 delta-1 and alpha-2 delta-2. Unchecked, these two proteins normally increase after an event such as a stroke or brain injury, inhibiting the brain’s ability to re-route lost function.
According to previous research by the same team, gabapentin blockade of alpha-2 delta-1 and alpha-2 delta-2 can prevent their normal inhibitory function, effectively lifting the brakes and enabling nerves to grow and regenerate lost function.
The brain “needs these subunits to be there,” said Dr. Tedeschi, but after a stroke, “they’re setting up the stage to create more excitability across the large area of the neural network and this contributes to the establishment of detrimental conditions.”
“Most of the time,” he said, “what we see is that under conditions where there is some form of plasticity, excitability of networks tends to be suppressed.”
When a neuron is hyperexcitable, it responds to a lower-than-normal stimulus threshold.
Dr. Tedeschi provided an example: “If you put your hands on a hard surface, you’re not supposed to feel pain because you feel like there is a hard surface under your hand. If somehow the signal now is miswired and there is hyperexcitability of the group of neurons that are controlling this mechanical sensation, this information is perceived as a painful stimulus.”
“When there is out-of-control neuronal excitability, then these neurons will respond to a very light, very low threshold input and that can cause muscle contraction even when you don’t want it,” said Dr. Tedeschi.
Spontaneous seizures, pain, and muscle spasms are causally linked to hyperexcitability.
The researchers induced ischemal stroke changes in the sensory-motor cortex of male and female mice using a photothrombotic stroke techniqueTrusted Source.
For the mice in the 6-week study who received daily gabapentin, the researches saw a significant recovery of motor control by the end of the study period.
Encouragingly, 2 weeks after treatment with gabapentin ceased, the mice retained that degree of improvement. The untreated mice did not recover motor control to the same extent.
As to whether the recovery of this degree of motor control was the extent of improvement mice may experience after gabapentin, Dr. Tedeschi noted with optimism:
“Yeah, certainly there’s going to be more beneficial effect than what we discover. And this is actually a work in progress. We are trying to dig deeper, and on a daily basis, we are actually discovering new things. This is something that unfortunately, I’m not allowed to discuss, but certainly, there are going to be follow-up studies. Pretty much like every week, we learn new things about the action of these drugs.”
Not all of gabapentin’s effects are positive, Dr. Tedeschi cautioned, meaning that there will likely be situations in which gabapentin would not be indicated.
Dr. Michael W. O’Dell, professor of clinical rehabilitation medicine at Weill Cornell Medicine in New York City, who was not involved in the study, told MNT: “There are always limitations in translating basic science, animal studies to humans, but in so much as this is a well-conducted study it does provide additional insights into the potential of pharmacological enhancement of brain plasticity in humans following stroke.”
“It should be pointed out, however, that in practice, in well-designed, larger clinical trials, there has not been a great deal of success in this area,” he noted.
“From a clinical standpoint,” Dr. O’Dell, added, “the fact that gabapentin is a widely available, inexpensive, and relative safe drug is an encouraging aspect of this study should the finding translate to any degree to a human population.”
Anticonvulsant Drug May Boost Functional Recovery after a Stroke
Scientists at the Ohio State University report that gabapentin, currently prescribed to control seizures and reduce nerve pain, may enhance recovery of movement after a stroke by helping neurons on the undamaged side of the brain take up the signaling work of lost cells.
Their study (“Harnessing cortical plasticity via gabapentinoid administration promotes recovery after stroke”), carried out in mice and published in Brain, mimicked ischemic stroke in humans, which occurs when a clot blocks blood flow and neurons die in the affected brain region. Results showed that daily gabapentin treatment for six weeks after a stroke restored fine motor functions in the animals’ upper extremities. Functional recovery also continued after treatment was stopped, the researchers found.
“Stroke causes devastating sensory-motor deficits and long-term disability due to disruption of descending motor pathways. Restoration of these functions enables independent living and therefore represents a high priority for those afflicted by stroke. Here, we report that daily administration of gabapentin, a clinically approved drug already used to treat various neurological disorders, promotes structural and functional plasticity of the corticospinal pathway after photothrombotic cortical stroke in adult mice,” the investigators wrote.
“We found that gabapentin administration had no effects on vascular occlusion, hemodynamic changes, nor survival of corticospinal neurons within the ipsilateral sensory-motor cortex in the acute stages of stroke. Instead, using a combination of tract tracing, electrical stimulation, and functional connectivity mapping, we demonstrated that corticospinal axons originating from the contralateral side of the brain in mice administered gabapentin extend numerous collaterals, form new synaptic contacts and better integrate within spinal circuits that control forelimb muscles.
“Not only does gabapentin daily administration promote neuroplasticity, but it also dampens maladaptive plasticity by reducing the excitability of spinal motor circuitry. “In turn, mice administered gabapentin starting one hour or one day after stroke recovered skilled upper extremity function. Functional recovery persists even after stopping the treatment at six weeks following a stroke.
“Finally, chemogenetic silencing of cortical projections originating from the contralateral side of the brain transiently abrogated recovery in mice administered gabapentin, further supporting the conclusion that gabapentin-dependent reorganization of spared cortical pathways drives functional recovery after stroke. These observations highlight the strong potential for repurposing gabapentinoids as a promising treatment strategy for stroke repair.”
Gabapentin found to block protein activity
The Ohio State University team previously found that gabapentin blocks the activity of a protein that, when expressed at elevated levels after an injury to the brain or spinal cord, hinders re-growth of axons, the long, slender extensions of nerve cell bodies that transmit messages.
“When this protein is high, it interferes with neurological recovery,” said lead author Andrea Tedeschi, PhD, assistant professor of neuroscience, in the Ohio State’s College of Medicine.
“Imagine this protein is the brake pedal, and recovery is the gas pedal. You can push on the gas pedal but can’t accelerate as long as you’re also pushing on the brake pedal,” Tedeschi said. “If you start lifting the brake pedal and continuously press on the gas, you can really speed up recovery. We think that is gabapentin’s effect on neurons, and there is a contribution of non-neuronal cells that tap into this process and make it even more effective.”
This work builds upon a 2019 study in which Tedeschi’s lab found in mice that gabapentin helped restore upper limb function after a spinal cord injury.
The primary treatment focus after an ischemic stroke is re-establishing blood flow in the brain as quickly as possible, but this research suggests that gabapentin has no role at that acute stage: The recovery results were similar whether the treatment started one hour or one day after the stroke.
Instead, the drug’s effects are evident in specific motor neurons whose axons carry signals from the central nervous system to the body that tell muscles to move.
After the stroke in study mice, the researchers observed, that neurons on the undamaged, or contralateral, side of the brain began sprouting axons that restored signals for upper extremity voluntary movement that had been silenced by neuron death after the stroke. This is an example of plasticity, the central nervous system’s ability to fix damaged structures, connections, and signals.
“The mammalian nervous system has some intrinsic ability to self-repair,” said Tedeschi, also a member of the Ohio State’s Chronic Brain Injury Program. “But we found this increase in spontaneous plasticity was not sufficient to drive recovery. The functional deficits are not so severe in this experimental model of ischemic stroke, but they are persistent.”
Because a technique that temporarily silenced the new circuitry reversed behavioral signs of recovery, Tedeschi said the findings suggested the drug normalizes conditions in the damaged nervous system to promote cortical reorganization in a functionally meaningful way.
Compared to control mice that did not receive the drug, mice that received six weeks of daily gabapentin treatment regained fine motor function in their forelimbs. Two weeks after treatment was stopped, researchers observed, functional improvements persisted.
“This confirmed that functional changes are solidified in the nervous system,” Tedeschi said.
Gabapentin also appeared to have an effect in the stroke-affected brain on non-neuron cells that influence the timing of message transmission. An examination of their activity after the drug treatment suggested these cells can dynamically change their behavior in response to variations in synaptic communication, further enabling smooth sprouting of axons that were compensating for the lost neurons.
The team is continuing to study the mechanisms behind stroke recovery, but Tedeschi said the findings suggest gabapentin holds promise as a treatment strategy for stroke repair. source
This already-approved drug could help repair the brain after stroke
hio State scientists have discovered that an already approved and widely prescribed drug, called gabapentin, may help the brain repair itself after a stroke.
Gabapentin is currently used to control seizures and help manage nerve pain, but in mice with blood clot-induced strokes, the drug helped the animals regain fine motor control in their upper limbs, with lasting improvement even after the treatment ended.
The discovery builds off of previous research, where the investigators learned that gabapentin blocks a protein in the brain that can hinder healing.
Over 600,000 people suffer a first stroke per year.
“When this protein is high, it interferes with neurological recovery,” Andrea Tedeschi, assistant professor of neuroscience at Ohio State, said in a statement.
He compared the protein to a brake pedal in a car. If you’re jamming down on the brake, you won’t go too far, no matter how hard you push on the gas pedal.
“If you start lifting the brake pedal and continuously press on the gas, you can really speed up recovery,” Tedeschi said. “We think that is gabapentin’s effect on neurons, and there is a contribution of non-neuronal cells that tap into this process and make it even more effective.”
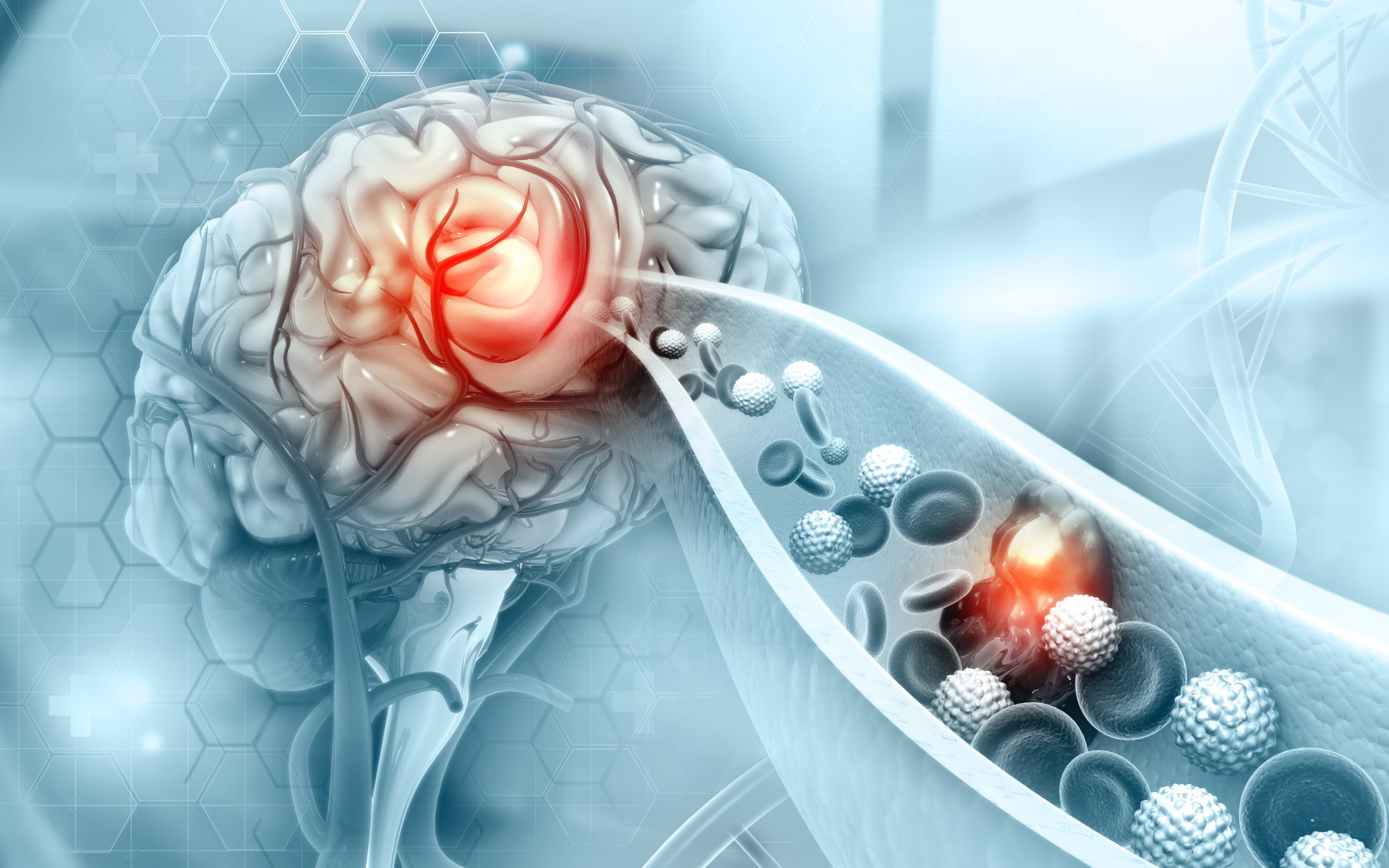
Stroke recovery: An ischemic stroke is caused by a clot choking off blood supply to part of the brain, leading to the death of brain cells in the impacted region.
This can lead to long term complications, including loss of muscle use, difficulty talking and swallowing, and emotional and memory issues.
According to the CDC, over 600,000 people suffer a first stroke each year, which means millions of people will need help recovering in the next few years alone.
Scientists have discovered that an already approved and widely prescribed drug, called gabapentin, may help the brain repair itself after a stroke.
The natural repair system: The first level treatment for ischemic stroke is to re-establish blood flow as quickly as possible, but the researchers found that this crucial step had no impact on gabapentin’s effectiveness, with motor function improvement happening whether the mice received the drug an hour or a day after stroke onset.
After the mice suffered a stroke, the neurons responsible for sending signals to the muscles from the undamaged sides of their brains began sprouting axons to form new connections, something popularly referred to as “plasticity” — the ability of different parts of the brain to adapt and repair damaged circuits and structures.
“The mammalian nervous system has some intrinsic ability to self-repair,” Tedeschi said, but not enough.
Injured neurons may become “hyperexcited,” firing signals that can cause muscle contractions and pain. If a brain protein called alpha2delta2 is expressed too much after a damaging incident like a stroke, it can contribute to this condition, while also slowing down axon growth.
A better fix: Gabapentin inhibits this protein, allowing the nerve cells to regrow and reorganize more efficiently and effectively.
“We blocked the receptor with the drug and asked, will even more plasticity occur? The answer is yes,” Tedeschi said.
Gabapentin restored forelimb motor control in mice.
Mice that received gabapentin daily for six weeks regained fine motor control in their forelimbs, which lasted for up to two weeks after dosing stopped; control mice who did not receive gabapentin did not regain motor control.
While a far cry from a sure thing in humans, the researchers believe that their study could be a first step towards finding a new use for an already-approved drug. Because the drug is already so widely used and understood, trials in humans may be faster and easier than for new drugs.
“These observations highlight the strong potential for repurposing gabapentinoids as a promising treatment strategy for stroke repair,” they wrote. source
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at tips@freethink.com.